Cataract
Add-On IOLs Bring Added Benefits
Primary and secondary implantation procedures offer advantages to alternatives.

Cheryl Guttman Krader
Published: Thursday, March 2, 2023
“ Published data from clinical and cadaver eye studies show the add-on IOLs are associated with good refractive outcomes and safety profiles. “
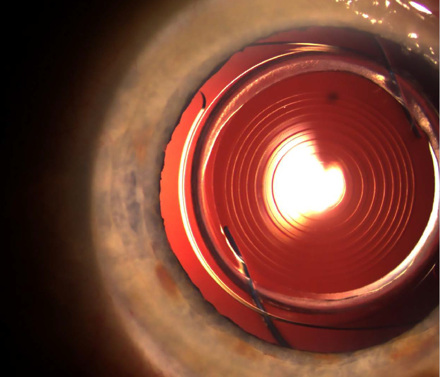
Supplementary (“add-on”) IOLs designed for implantation into the sulcus provide a reversible solution for refractive enhancement after cataract surgery or when implanted during the primary surgery in a “duet” procedure to correct presbyopia, Oliver Findl MD told a recent conference.
Polypseudophakia was first described in 1993 and involved piggybacking a second standard IOL in the capsular bag to treat high hyperopia. However, postoperative problems such as interlenticular membrane formation—with opacification and hyperopic defocus—meant a second IOL placement into the ciliary sulcus. But this technique was done using an IOL intended for implantation in the capsular bag, which resulted in complications including pigment dispersion, inflammation, elevated IOP, and haemorrhage.
“The idea then emerged to design an IOL optimised for sulcus implantation into the pseudophakic eye,” Dr Findl explained.
Currently, there are three commercially available add-on IOL models for refractive indications: Reverso (Cristalens), Sulco flex (Rayner), and 1stQ AddOn (Medicontour). All are made of biocompatible hydrophilic acrylic and feature a 6.5-mm optic that gives good overlap with the IOL in the bag while avoiding iris optic capture. In addition, they have round optic edges to minimise dysphotopsia risk, a concave posterior surface to avoid contact with the IOL in the bag, and haptics designed to provide good centration, rotational stability, and uveal clearance. Available optic designs include aspheric monofocal, refractive and diffractive multifocal, toric, and multifocal toric.
Published data from clinical and cadaver eye studies show the add-on IOLs are associated with good refractive outcomes and safety profiles. A study of the Sulcoflex IOL showed its centration was better than that of the in-the-bag IOL. A bench study comparing optical quality of a single trifocal in-the-bag IOL with a trifocal add-on IOL plus an in-the-bag monofocal IOL found no difference between the two systems.
Consistent with the good visual outcomes, studies evaluating the add-on IOLs also show good and stable centration. However, a study of eyes implanted with a toric add-on IOL found rotation in 10% of cases.
“A toric add-on IOL can be suture fixated in the sulcus. However, this is a little tricky, and surgeons would prefer not to have to do that,” Dr Findl said.
Surgical planning and performance
In cases of secondary implantation to correct postoperative ametropia ±7.0 D of target, the IOL power calculation is simple as the patient’s current refraction can serve as the base, he noted. The patient’s spherical equivalent is multiplied by 1.5 in cases of hyperopia or by a factor of 1.2 for myopia. The R-vergence formula, which incorporates values for keratometry and anterior chamber depth in addition to the spherical equivalent, can serve as an alternative.
Dr Findl observed implanting the add-on IOL is also straightforward. In a duet procedure, after the primary IOL is implanted into the bag and viscoelastic removed from inside the capsule bag, more viscoelastic is placed under the iris to open the sulcus. An injector or forceps delivers the add-on IOL through a 2.4-mm or slightly smaller incision. Once positioned, viscoelastic is aspirated, with special attention directed to removing the material from the interface between the two lenses.
Implanting an add-on IOL in a secondary procedure to correct ametropia or explanting or exchanging an existing add-on IOL are also easier and less risky procedures than exchanging an IOL in the capsular bag.
“If a patient with a multifocal add-on IOL is troubled early on by dysphotopsia or a lack of neuroadaptation, surgeons simply need to reopen the incision and remove the lens,” Dr Findl said. “The add-on lens can also be easily removed years later if needed because of pathological changes, such as the development of age-related macular degeneration or diabetic macular oedema.”
Dr Findl presented during the AAO 2022 Refractive Surgery Subspecialty Day meeting in Chicago, US. He spoke on behalf of Michael Amon MD, PhD, Vienna, Austria, inventor of a commercially available add-on IOL platform.
Oliver Findl MD is the Chair of the Department of Ophthalmology, Hanusch Hospital, Vienna, Austria. He is current president of the ESCRS. oliver@findl.at
Michael Amon MD, PhD is Head of the Department of Ophthalmology Academic Teaching Hospital of St. John Chair for Ophthalmology at Sigmund Freud Private-University in Vienna, Austria. amon@augenchirurg.com
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.